TMS for Stroke: A Revolutionary Approach to Post-Stroke Recovery
Stroke is a leading cause of long-term disability and affects millions of individuals each year. Recovery is often slow and complex, involving physical, cognitive, and emotional challenges. Traditional rehabilitation methods such as physical therapy and speech therapy remain essential, but in recent years, Transcranial Magnetic Stimulation (TMS) has emerged as a groundbreaking adjunct therapy for stroke recovery.
TMS For Stroke is transforming the way we approach rehabilitation by tapping into the brain’s ability to rewire itself. In this article, we will explore how TMS works, its benefits for stroke patients, safety considerations, clinical evidence, and what patients can expect from treatment.
What Is Transcranial Magnetic Stimulation (TMS)?
Transcranial Magnetic Stimulation (TMS) is a non-invasive brain stimulation technique that uses magnetic fields to stimulate nerve cells in specific areas of the brain. It involves placing a magnetic coil near the scalp to deliver short bursts of magnetic energy to the targeted region. These pulses activate neurons and help modulate brain activity.
Initially approved for treatment-resistant depression, TMS is now being studied and applied in neurological rehabilitation, including stroke recovery.
Understanding Stroke and Its Aftermath
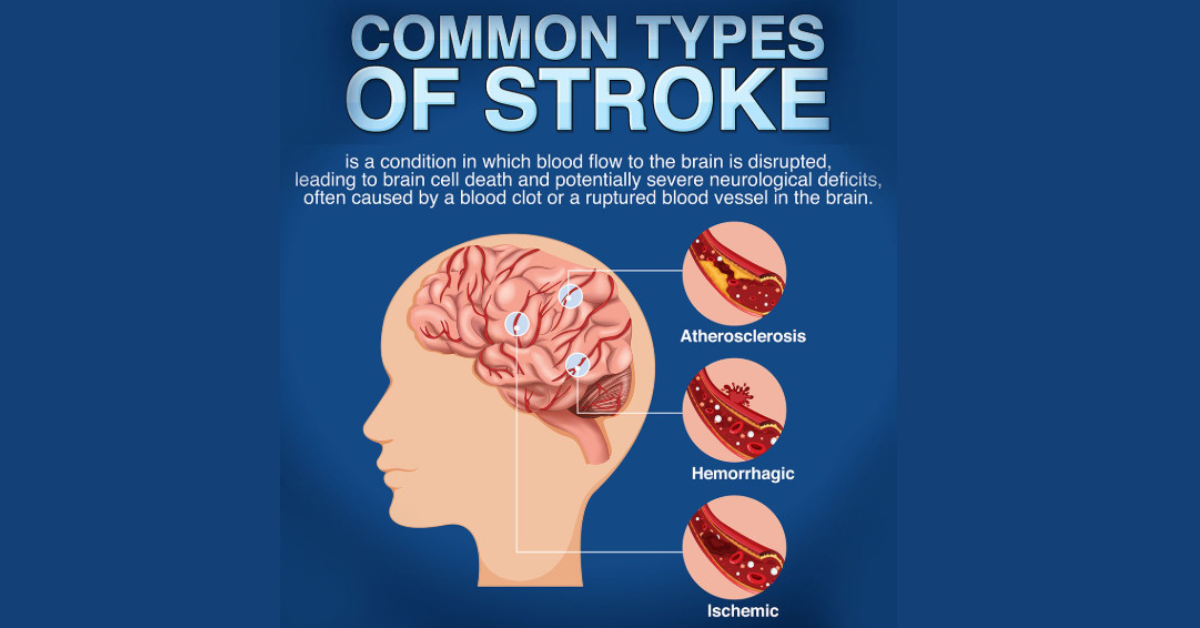
A stroke occurs when the blood supply to a part of the brain is interrupted, either due to a clot (ischemic stroke) or a rupture (hemorrhagic stroke). This disruption can lead to brain damage, which often results in:
-
Paralysis or weakness (often on one side of the body)
-
Speech and language impairments (aphasia)
-
Cognitive challenges such as memory loss or attention deficits
-
Difficulty with balance and coordination
-
Depression or emotional changes
Recovery depends on the brain’s ability to adapt and reorganize itself — a phenomenon known as neuroplasticity. TMS plays a key role in enhancing this natural process.
How TMS Aids in Stroke Recovery
TMS enhances stroke rehabilitation by directly stimulating the brain’s neural networks. Here’s how it contributes to the recovery process:
1. Promotes Neuroplasticity
TMS increases the brain’s capacity to form new neural pathways. This is crucial for relearning skills lost after a stroke, such as walking or speaking.
2. Rebalances Brain Activity
Stroke can cause an imbalance between the damaged and healthy sides of the brain. For example, the unaffected hemisphere may become overactive and suppress recovery in the affected hemisphere. TMS helps restore balance by either exciting the damaged side or inhibiting the overactive side.
3. Improves Motor Function
When TMS is applied to the motor cortex, it can improve movement in the limbs, particularly in the hand and arm. Studies show that repetitive TMS (rTMS) can enhance voluntary movement and coordination.
4. Supports Speech and Language Recovery
Patients with aphasia (speech difficulties) may benefit from TMS targeting language-processing areas of the brain. Some clinical trials have demonstrated improved word retrieval and fluency.
5. Reduces Post-Stroke Depression
Depression is common after a stroke and can interfere with rehabilitation. TMS is FDA-approved for depression and can significantly improve mood, motivation, and overall mental health in stroke survivors.
Clinical Evidence for TMS in Stroke Rehabilitation
Numerous clinical studies support the use of TMS for stroke rehabilitation:
-
A study in The Lancet Neurology reported that rTMS led to significant improvement in hand function among chronic stroke patients.
-
Research in Stroke: A Journal of Cerebral Circulation showed that low-frequency TMS applied to the unaffected hemisphere can reduce its inhibitory effect on the damaged side, promoting better motor recovery.
-
In patients with non-fluent aphasia, TMS applied to the right hemisphere has shown promise in improving language abilities.
These studies suggest that TMS, when integrated with conventional therapy, can lead to improved outcomes for many stroke survivors.
What Happens During a TMS Treatment Session?
TMS is typically administered in an outpatient setting and does not require anesthesia or recovery time. Here’s what a typical session looks like:
Initial Evaluation
Patients undergo a full assessment to determine eligibility and the appropriate brain areas for stimulation. This may involve neuroimaging, clinical exams, and cognitive testing.
During the Session
-
The patient sits in a reclining chair.
-
A magnetic coil is placed on the scalp, aligned with the treatment target (e.g., motor cortex, language areas).
-
Magnetic pulses are delivered for 20–40 minutes.
-
The patient remains awake and alert.
Treatment Schedule
Most patients receive TMS five days a week for four to six weeks. Some may require maintenance sessions depending on their progress and condition.
Who Can Benefit from TMS After a Stroke?
TMS may benefit individuals who:
-
Have persistent motor deficits despite standard rehabilitation
-
Experience post-stroke depression
-
Struggle with cognitive impairments or speech difficulties
-
Are medically stable and cleared by their physician
TMS is most effective when started within the subacute (weeks to months) or chronic phase (months to years) after a stroke. However, early interventions are also being studied.
Safety and Side Effects
TMS is generally considered safe, especially when administered by trained professionals.
Common Side Effects
-
Mild headache
-
Scalp discomfort
-
Tingling or muscle twitching during treatment
Rare Side Effects
-
Seizures (extremely rare, especially when safety guidelines are followed)
-
Dizziness or lightheadedness
Patients with a history of seizures, metal implants in the head, or certain medical conditions should undergo careful screening before starting TMS.
Integrating TMS With Traditional Stroke Rehabilitation
TMS is not a replacement for conventional therapy but rather a powerful supplement. It is often integrated with:
-
Physical therapy: TMS can enhance motor learning and muscle control.
-
Speech therapy: It can help re-engage language centers in the brain.
-
Occupational therapy: TMS supports improved coordination and fine motor skills.
This integrative approach provides the best chance for functional recovery.
TMS for Stroke: Real-World Results
Stroke survivors who undergo TMS often report:
-
Improved movement in affected limbs
-
Increased speech fluency and comprehension
-
Enhanced cognitive abilities such as memory and attention
-
Reduced feelings of depression or anxiety
-
Greater motivation to engage in therapy
While not a cure, TMS can significantly improve quality of life and rehabilitation outcomes when used in a structured, multidisciplinary setting.
Frequently Asked Questions (FAQs)
1. Is TMS FDA-approved for stroke rehabilitation?
TMS is FDA-approved for depression but is used off-label for stroke rehabilitation. It is widely supported by clinical research and used in many leading medical centers.
2. How soon after a stroke can TMS begin?
TMS can begin a few weeks after a stroke, especially once the patient is medically stable. The ideal timing depends on individual recovery progress and physician recommendations.
3. How many sessions are needed?
Most treatment plans include 20–30 sessions over 4–6 weeks. Some patients may benefit from additional sessions or maintenance therapy.
4. Can TMS be combined with other treatments?
Yes. TMS works best when combined with physical, speech, and occupational therapy. It enhances the brain’s responsiveness to these traditional approaches.
5. Is TMS covered by insurance for stroke patients?
While TMS is commonly covered for depression, insurance coverage for stroke rehabilitation varies. Patients should check with their provider for specific benefits.
Conclusion
TMS for stroke is ushering in a new era of neurorehabilitation. By stimulating the brain’s natural healing mechanisms, TMS helps stroke survivors regain function, improve mood, and reclaim independence. While it is not a standalone solution, it is an effective addition to comprehensive stroke care.
At TMS Psychiatry and Medical (tmspm.com), we are committed to offering advanced, evidence-based solutions for stroke recovery. If you or a loved one is navigating the challenges of post-stroke rehabilitation, consider exploring whether TMS is the right step forward.